Authors
Rimda Wanchoo, Leonardo V. Riella, Nupur N. Uppal, Carlos A. Lopez, Vinay Nair, Craig Devoe, Kenar D. Jhaveri
Abstract
The use of immune checkpoint inhibitors (ICI) in several cancers is expanding; however, their use in patients with cancer and an organ transplant is very limited. In this review, we summarize the literature and the experience of anti-cytotoxic T-lymphocyte-associated protein 4 (CTLA-4) and anti-programmed cell death protein 1 (PD-1) inhibitors in the organ transplant patient. The immunology of CTLA-4 and PD-1 inhibitors and their role in tolerance breakdown is also reviewed. While CTLA-4 inhibitors have been successfully used in kidney, liver, and heart transplant patients without rejection, the uses of PD-1 inhibitors and the combination therapy of CTLA-4 and PD-1 inhibitors have been associated with cellular- and antibody-mediated rejection. While immunosuppression minimization is needed for ICI to provide the best response when managing transplant patients who develop malignancy, this can lead to rejection episodes. Prevention strategies, such as the use of ongoing steroids and sirolimus, could prevent rejection while sustaining tumor response. As the experience grows with these agents, we will learn more about tolerance and the use of ICI in the organ transplant patient. Therefore, the use of an immune checkpoint blockade in transplantation is extremely difficult, and future research should focus on finding the right balance between unleashing the immune system to provide an anti-tumor effect but at the same time sustaining tolerance so that rejection is suppressed. Also, the ability to identify biomarkers that may predict rejection early and allow for the fine tuning of doses and frequencies of drug administration would be very helpful.
http://www.onconephrologyjournal.com/article/9110d873-b60a-43a8-be6e-25fcaa6dd341
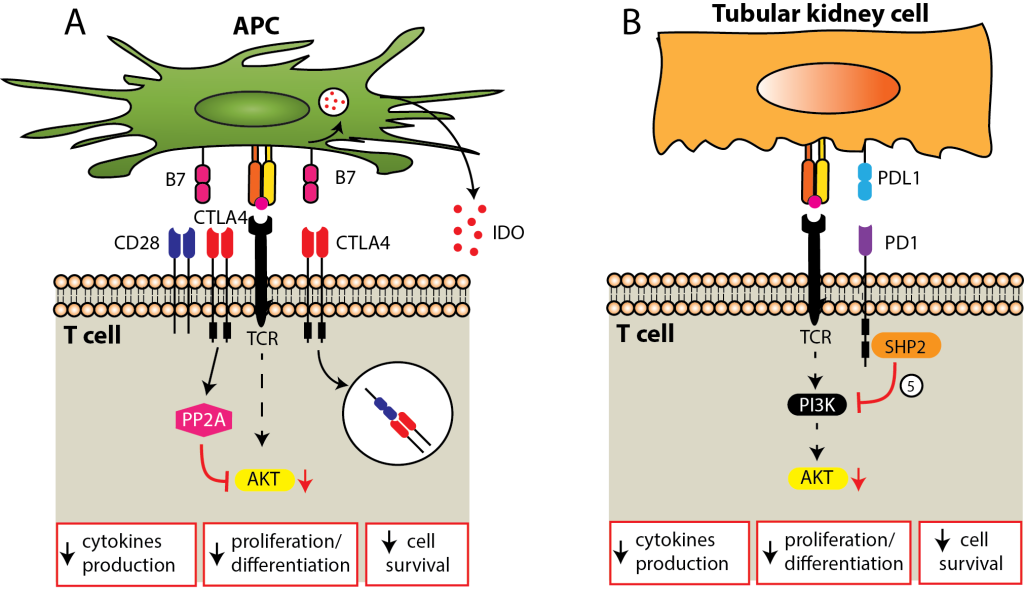
Co-inhibitory signals. (A) CTLA-4 signal may inhibit T cells through multiple mechanisms, including competition with CD28 for B7 ligands, inhibition of intracellular signal downstream from the TCR, internalization of B7 ligands, or the release of indoleamine 2,3-dioxygenase (IDO) by the APC. (B) PD1 signal inhibits T cell by recruiting tyrosine phosphatase SHP-2, which then inactivates PI3K, a critical step in T cell activation. While CTLA-4 signals predominate on secondary lymphoid organs, PD-1 is dominant on the peripheral target tissue, such as tubular epithelial kidney cells. APC = antigen-presenting cell; CTLA-4 = anti-cytotoxic T-lymphocyte-associated protein 4; PD-1 =anti-programmed cell death protein 1; TCR = T cell receptor.