Am J Transplant. 2019 Jul 25. doi: 10.1111/ajt.15545.
Authors
Li GZ, Tio MC, Pak LM, Krier J, Seifter JL, Tullius SG, Riella LV, Malek SK, Stergachis AB.
Abstract
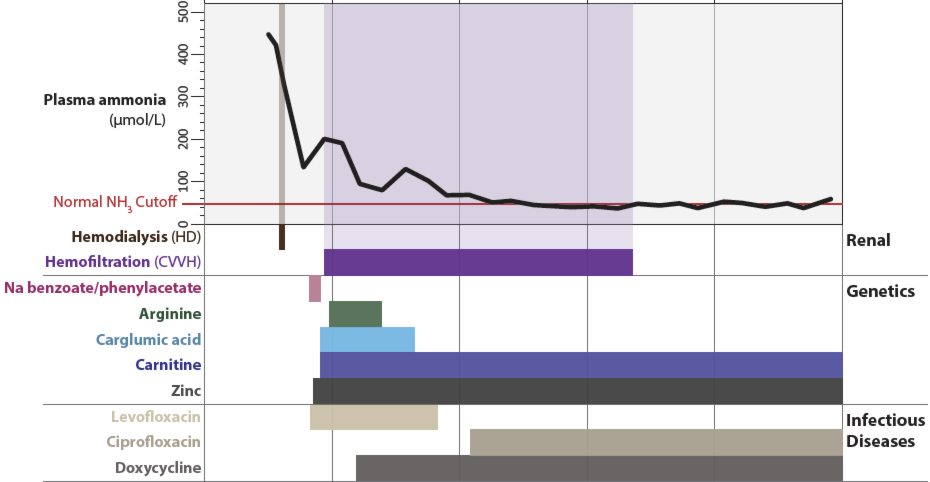
A 72-year-old woman with end-stage kidney disease due to recurrent urinary tract infections and obstructive uropathy of a solitary kidney presented to our hospital for renal transplantation. She underwent successful transplantation of a deceased donor allograft, but developed acute mental status deterioration on the fifth postoperative day. Her serum ammonia was found to be markedly elevated to 447 μmol/L in the setting of normal hepatic function. She was treated with emergent dialysis and empiric antibiotics targeting urea-splitting organisms, and ultimately made a full neurologic recovery with stable renal allograft function. Noncirrhotic hyperammonemia (NCH) is an exceedingly rare clinical entity but seems to have a predilection for patients who have undergone solid organ transplantation. This report emphasizes the importance of rapid diagnosis and initiation of treatment for NCH, which is associated with a high rate of mortality and irreversible neurological morbidity. We outline the successful workup and management approach for this patient.
Figure 1. Clinical presentation, evolution and management of hyperammonemia in the case presented.