Abstract
The incidence of malignancy is greater in kidney transplant recipients compared to the general population, though the higher risk is not equally distributed to all types of cancers. In face of the increased longevity of renal transplant recipients, certain cancers, such as acute leukemias, are becoming more prevalent. Acute myeloid leukemia (AML) typically presents with cytopenias and infections, both common findings after kidney transplantation. Therefore, the diagnosis of AML may be initially overlooked in these patients. We report the case of a 33-year-old man who presented with fever, pancytopenia and acute worsening of his renal allograft function 9 years after a living unrelated kidney transplant. After initial negative infectious work-up, a kidney biopsy revealed C4d-positive antibody-mediated rejection in combination with scattered atypical inflammatory cells. A subsequent bone marrow biopsy confirmed AML. He underwent successful induction chemotherapy with daunorubucin and cytarabine and ultimately achieved a complete remission. However, he developed a Page kidney with worsening renal function and abdominal pain three weeks after biopsy in the setting of chemotherapy-induced thrombocytopenia. Herein, we discuss the prevalence, risk factors, presentation and management of leukemia after kidney transplantation.
Acute myeloid leukemia after kidney transplantation: a case report and literature review.
Cardarelli F, Bijol V, Chandraker A, Varga C, Riella LV.
J Bras Nefrol. 2016 Dec;38(4):455-461. doi: 10.5935/0101-2800.20160072. Portuguese, English.
- PMID: 28001189
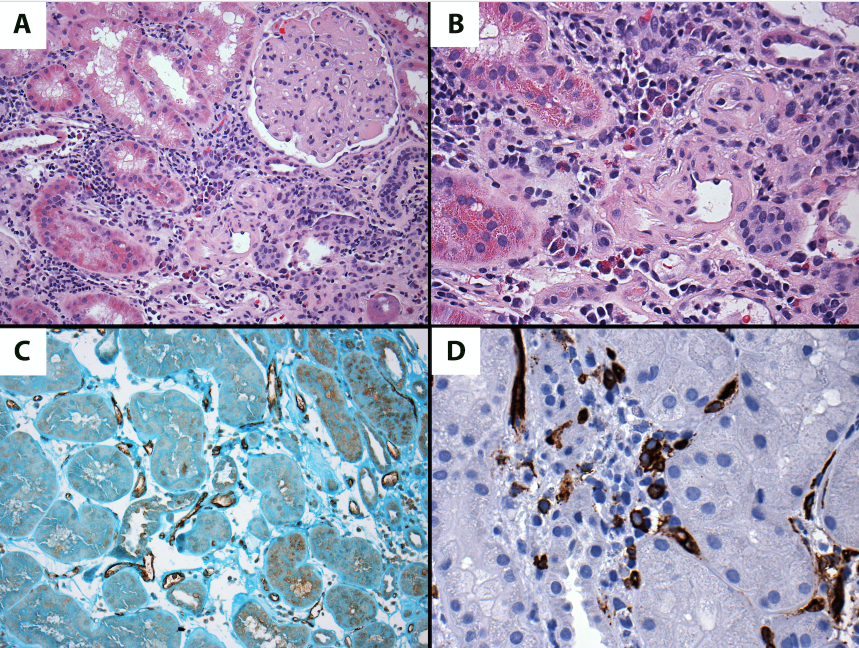
Light microscopy of the kidney biopsy, representative images; (A) Glomerulus with mesangial expansion and capillary wall remodeling and thickening, consistent with transplant glomerulopathy (H&E, 200X). In addition, focal inflammatory infiltrate is noted, better appreciated on (B), with mixed infiltrate with frequent eosinophils, lymphocytes and atypical inflammatory cells (H&E, 400X). (C) The C4d stain is positive circumferentially along the peritubular capillaries (C4d, immunoperoxidase stain, 400X) (D) The CD34-positive blast forms are seen frequently within the interstitial infiltrate (CD34, immunoperoxidase stain, 400X).