Am J Transplant. 2018 Oct 12. doi: 10.1111/ajt.15143. [Epub ahead of print]
Authors:
Krezdorn N, Lian CG, Wells M, Wo L, Tasigiorgos S, Xu S, Borges TJ, Frierson RM, Stanek E, Riella LV, Pomahac B, Murphy GF.
Abstract:
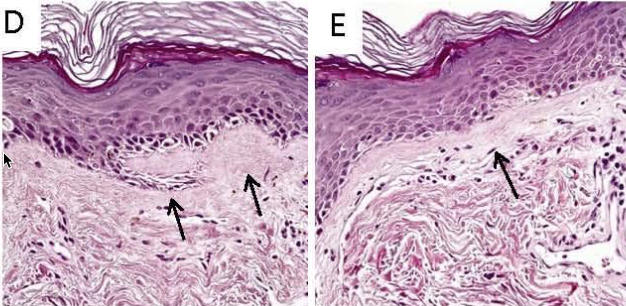
Face vascularized composite allografts (FVCA) have helped severe patient disfigurement, with acute rejection now largely controlled through iatrogenic immunosuppression. However, little is known regarding the incidence and mechanism(s) of more long-term pathologic alterations in FVCAs that may affect function and graft durability. Protocol surveillance biopsies for up to an 8 year interval in seven patients who received FVCAs at our institution revealed histopathologic evidence of chronic rejection. Clinical manifestations included features of premature aging, mottled leukoderma accentuating suture lines, telangiectasia, and dryness of nasal mucosa. Pathologic changes consisted of epidermal thinning accompanied by discrete foci of lymphocyte-mediated cytotoxicity, hyperkeratosis, follicular plugging, vascular ectasia, and sclerosis beneath the epidermal layer associated with collagen type I deposition. Genomic interrogation and immunohistochemistry of sclerotic zones revealed upregulation of the AP-1 pathway components, JunB and c-Fos, previously implicated in overproduction of type I dermal collagen in the setting of systemic sclerosis. We conclude that some patients develop chronic rejection in FVCAs with striking similarities to alterations seen in certain autoimmune cutaneous disorders (lupus erythematosus and scleroderma/chronic sclerodermoid GVHD). Identification of relevant pathways and genes, such as JunB and c-Fos, may provide new targets into preventative therapies for chronic immune-mediated changes in vascularized composite allografts.
Figure 1D,E: Evidence of chronicity in face transplant biopsies. Fibrous thickening of subepidermal basement membrane zones.