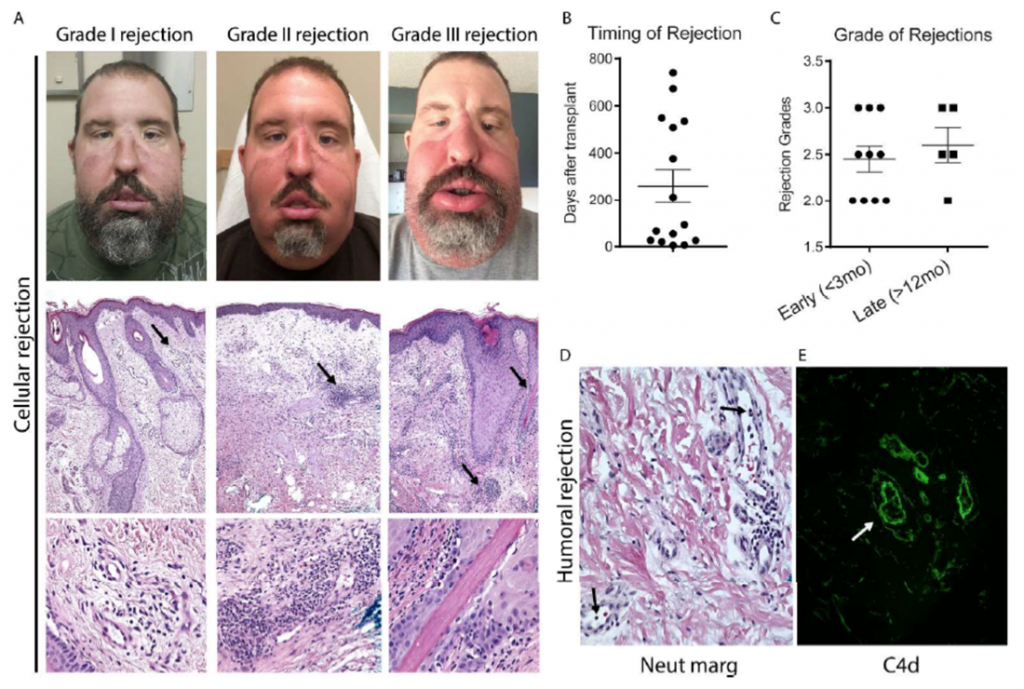
Facial transplantation is a life-changing procedure for patients with severe composite facial defects. However, skin is the most immunogenic of all transplants and better understanding of the immunological processes after facial transplantation is of paramount importance. Here, we describe six patients that underwent full facial transplantation in our institution, with a mean follow-up of 2.7 years. Serum, PBMCs and skin biopsies were collected prospectively and a detailed characterization of their immune response (51 time-points) was performed, defining 47 immune cell subsets, 24 serum cytokines, anti-HLA antibodies, and donor alloreactivity on each sample, producing 4,269 data points. In a non-rejecting state, patients had a predominant Th2 phenotype in the blood. All patients developed at least one episode of acute cellular rejection, which was characterized by increases in IFN-γ/IL-17-producing cells in peripheral blood and in the allograft’s skin. Serum MCP-1 level was significantly increased during rejection compared to pre-rejection time-points. None of the patients developed de novo donor-specific antibodies (DSA), despite a 4-fold expansion in T follicular helper cells at 1 year post-transplant. In sum, facial transplantation is frequently complicated by a co-dominant IFN-γ/IL-17-mediated acute cellular rejection process. Despite that, medium-term outcomes are promising with no evidence of de novo DSA development. This article is protected by copyright. All rights reserved.
Borges TJ , O’Malley JT, Wo L, Murakami N, Smith B, Azzi J, Tripathi S, Lane JD, Bueno EM, Clark RA, Tullius SG, Chandraker A, Lian CG, Murphy GF, Strom TB, Pomahac B, Najafian N, Riella LV. “Co-Dominant Role of IFN-γ- and IL-17-Producing T Cells During Rejection in Full Facial Transplant Recipients,” American Journal of Transplantation 2016 Jan 8.