 One controversial aspect in the evaluation of potential kidney recipients is the performance of stress tests for risk stratification. With the cost of stress tests ranging from U$2,500-5,000 and the long waiting time for a kidney transplant on the deceased donor list, this is a particular important point for financial, medical and logistical reasons. To evaluate that, De Lima et al. studied the prognostic value of myocardial scintigraphy in 892 consecutive renal transplant candidates classified into four risk groups: very high (aged ≥50 years, diabetes and cardiovascular disease), high (two factors), intermediate (one factor) and low (no factor). After a median follow up of 22 months, 181 major cardiovascular (CV) events were observed (overall incidence = 20%): 12 (6.6%) in low-risk, 51 (28.2%) in intermediate-risk, 61 (33.7%) in high-risk and 57 (31.5%) in very high-risk patients (p below 0.0001; Figure below). This simple classification was able to nicely separate the different groups according to incidence of major CV events.
One controversial aspect in the evaluation of potential kidney recipients is the performance of stress tests for risk stratification. With the cost of stress tests ranging from U$2,500-5,000 and the long waiting time for a kidney transplant on the deceased donor list, this is a particular important point for financial, medical and logistical reasons. To evaluate that, De Lima et al. studied the prognostic value of myocardial scintigraphy in 892 consecutive renal transplant candidates classified into four risk groups: very high (aged ≥50 years, diabetes and cardiovascular disease), high (two factors), intermediate (one factor) and low (no factor). After a median follow up of 22 months, 181 major cardiovascular (CV) events were observed (overall incidence = 20%): 12 (6.6%) in low-risk, 51 (28.2%) in intermediate-risk, 61 (33.7%) in high-risk and 57 (31.5%) in very high-risk patients (p below 0.0001; Figure below). This simple classification was able to nicely separate the different groups according to incidence of major CV events.
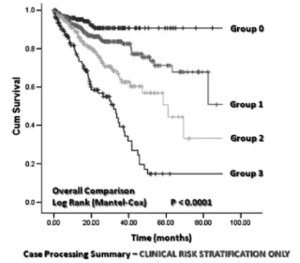 The prevalence of abnormal scan increased with the degree of risk, from 12.7% in low-risk patients to 50.8% among very high-risk subjects. Interestingly, only in patients with one risk factor (either age ≥50 years, diabetes or CV disease) was an altered myocardial stress test associated with an increased incidence of major CV events [30.3 versus 10%, hazard ratio (HR) = 2.37; p below 0.0001). Low-risk patients did well regardless of stress test results, while in patients with 2 or 3 risk factors, altered stress test did not add to the already increased risk for future CV events.
The prevalence of abnormal scan increased with the degree of risk, from 12.7% in low-risk patients to 50.8% among very high-risk subjects. Interestingly, only in patients with one risk factor (either age ≥50 years, diabetes or CV disease) was an altered myocardial stress test associated with an increased incidence of major CV events [30.3 versus 10%, hazard ratio (HR) = 2.37; p below 0.0001). Low-risk patients did well regardless of stress test results, while in patients with 2 or 3 risk factors, altered stress test did not add to the already increased risk for future CV events.
The question that remains is whether an invasive intervention could lower the CV events in the high-risk groups and if coronary angiography should be considered instead of stress test, as proposed by some. The cost, invasiveness and risk of the procedure would likely be unwarranted until a randomized trial show benefits of revascularization in ESRD pts compared to medical management. It is important to remember that most clinical trials addressing this question exclude ESRD patients so we must extrapolate data from the general population, which do not support intervention in asymptomatic patients. An upcoming randomized controlled trial is addressing this question in transplantation: COST trial.
Until then, we have to base our decisions on observational/restrospective data and poor evidence-based guidelines. My personal approach has been not to screen low risk patients with stress test anymore but I am still performing stress tests for selected intermediate and high-risk patients. The reason to do a stress test on a high risk patient is not to assess for the presence or not of CV disease, but to attempt to identify a large defect, exercise-induced hypotension or angina that might warrant intervention prior to transplantation. Among the stress tests, I usually recommend a MIBI protocol with sequential exercise followed by pharmacological (if HR goal not achieved), which allows for evaluation of patient’s exercise capacity and cardiac imaging to determine the burden of CV disease. For obese patients, PET may give you better images.
To provoke even more the debate, Diamond et al. supports the approach of: “test no one and treat everyone” for asymptomatic diabetic patients compared to “screen everyone and treat only those with an abnormal test”. The authors believe that optimal medical interventions such as statins/beta blocker are sometimes ignored after a normal stress test (high false negative rate), missing an important point of intervention, which could be more cost-effective than the screening strategy. One of the key concepts supporting this approach is that myocardial infarction tends to correlate with endothelial disease, and not the degree of obstruction of a coronary artery. Consequently, the sensitivity and specificity of any cardiovascular testing is somewhat problematic (meta-analysis by Want et al. Transp 2015). Also supporting the strategy of “treat all” is the work from Baiegent et al. using statin and ezetimibe in patients with advanced CKD (Lancet 2011). Definitely lots of fuel for more debate…
