Am J Transplant. 2023 Feb 4. doi: 10.1016/j.ajt.2023.01.016.Online ahead of print.
Authors:
Murakami N, Borges TJ, Win TS, Abarzua P, Tasigiorgos S, Kollar B, Barrera V, Ho Sui S, Teague JE, Bueno E, Clark RA, Lian CG, Murphy GF, Pomahac B, Riella LV.
Abstract:
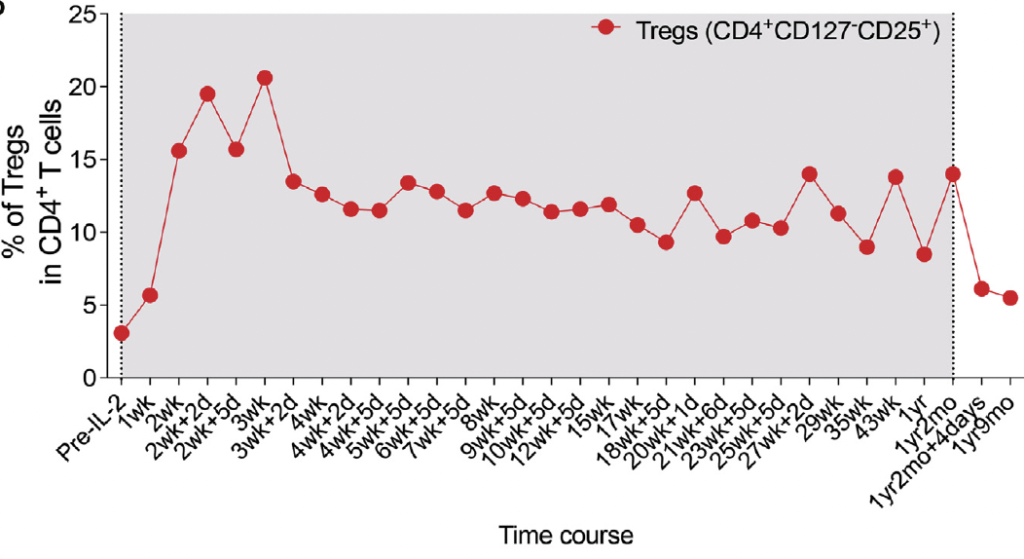
Face transplantation is a life-changing procedure for patients with severe composite facial defects. However, it is hampered by high acute rejection rates due to the immunogenicity of skin allograft and toxicity linked to high doses of immunosuppression. To reduce immunosuppression-associated complications, we, for the first time in face transplant recipients, used low-dose interleukin 2 (IL-2) therapy to expand regulatory T cells (Tregs) in vivo and to enhance immune modulation, under close immunological monitoring of peripheral blood and skin allograft. Low-dose IL-2 achieved a sustained expansion (∼4-fold to 5-fold) of circulating Tregs and a reduction (∼3.5-fold) of B cells. Post-IL-2 Tregs exhibited greater suppressive function, characterized by higher expression of TIM-3 and LAG3co-inhibitory molecules. In the skin allograft, Tregs increased after low-dose IL-2 therapy. IL-2 induced a distinct molecular signature in the allograft with reduced cytotoxicity-associated genes (granzyme B and perforin). Two complications were observed during the trial: one rejection event and an episode of autoimmune hemolytic anemia. In summary, this initial experience demonstrated that low-dose IL-2 therapy was not only able to promote immune regulation in face transplant recipients but also highlighted challenges related to its narrow therapeutic window. More specific targeted Treg expansion strategies are needed to translate this approach to the clinic.
Figure. Treg expansion during low-dose IL-2 treatment.