Braz J Nephrology. 2019 Oct-Dec;41(4):448-450.
Authors
Murakami N, Riella LV.
Abstract
Kidney transplantation is the treatment of choice for end-stage renal disease (ESRD). In the US, studies have shown a clear survival benefit of transplantation even when the recipients are HLAincompatible with positive cross-matches, compared with remaining on the waitlist1. However, organ shortage has been a universal challenge for the transplant field and the number of patients on the waitlist continues to rise. In order to expand the organ donor pool, several approaches have been taken, including kidney swap programs for sensitized patients or ABOincompatible living donor-recipient pairs. For deceased donors, the use of expanded criteria donors, transplantation from HCV-positive donors to HCV-negative recipients, and use of HIV-positive organs have been implemented. Despite these efforts, the organ discard rate isstill high at about 20% of all organoffers2, and the rate is higher in donors with acute kidney injury (AKI). The most common reason for turning down organ offers is the “inadequate” quality of the organs based on biopsy, followed by either AKI or expanded criteria donor with significant kidney risk factors. This tendency continues after incorporation of a new kidney allocation policy in the US in 2014. Therefore, it is of particular importance to determine long-term outcomes of recipients who received kidneys from AKI donors and to establish the risk factors for post-transplant kidney dysfunction.
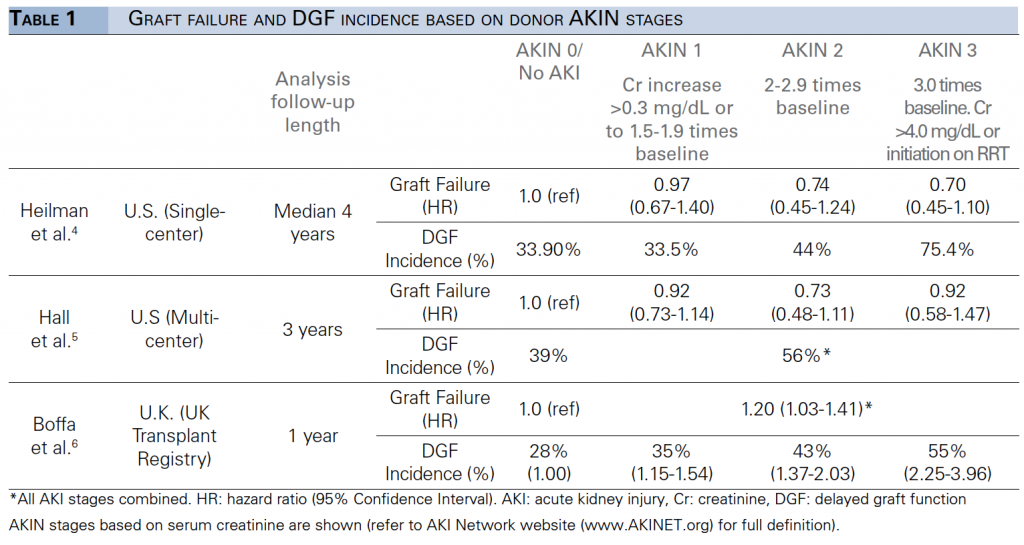
Table. Graft failure and DGF incidence based on donor AKIN stages.